Background: Chronic obstructive pulmonary disease (COPD) and asthma are considered as the two most widespread obstructive lung diseases, whereas they affect more than 500 million people worldwide. Unfortunately, the requirement for detailed geometric models of the lungs in combination with the increased computational resources needed for the simulation of the breathing did not allow great progress to be made in the past for the better understanding of inflammatory diseases of the airways through detailed modelling approaches. In this context, computational fluid dynamics (CFD) simulations accompanied by fluid particle tracing (FPT) analysis of the inhaled ambient particles are deemed critical for lung function assessment. Also they enable the understanding of particle depositions on the airways of patients, since these accumulations may affect or lead to inflammations. In this direction, the current study conducts an initial investigation for the better comprehension of particle deposition within the lungs. More specifically, accurate models of the airways obstructions that relate to pulmonary disease are developed and a thorough assessment of the airflow behavior together with identification of the effects of inhaled particle properties, such as size and density, is conducted. Our approach presents a first step towards an effective personalization of pulmonary treatment in regards to the geometric characteristics of the lungs and the in depth understanding of airflows within the airways.
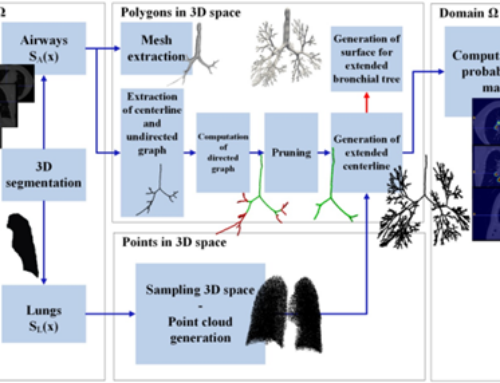
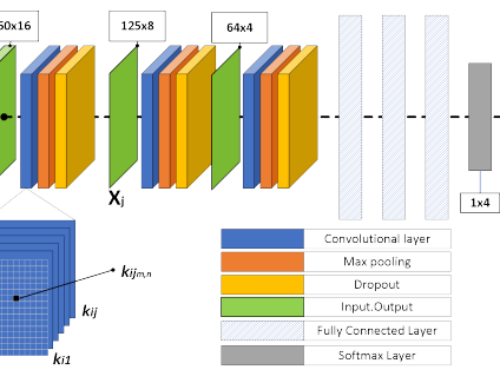
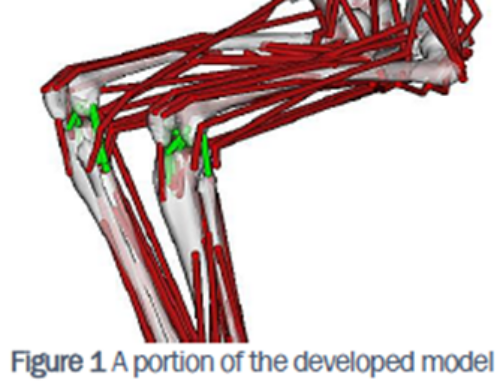
Methods: A geometry processing technique involving contraction algorithms is established and used to employ the different respiratory arrangements associated with lung related diseases that exhibit airways obstructions. Apart from the normal lung case, two categories of obstructed cases are examined, i.e. models with obstructions in both lungs and models with narrowings in the right lung only. Precise assumptions regarding airflow and deposition fraction (DF) over various sections of the lungs are drawn by simulating these distinct incidents through the finite volume method (FVM) and particularly the CFD and FPT algorithms. Moreover, a detailed parametric analysis clarifies the effects of the particles size and density in terms of regional deposition upon several parts of the pulmonary system. In this manner, the deposition pattern of various substances can be assessed. Results: For the specific case of the unobstructed lung model most particles are detected on the right lung (48.56% of total, when the air flowrate is 12.6 L/min), a fact that is also true when obstructions arise symmetrically in both lungs (51.45% of total, when the air flowrate is 6.06 L/min and obstructions occur after the second generation). In contrast, when narrowings are developed on the right lung only, most particles are pushed on the left section (68.22% of total, when the air flowrate is 11.2 L/min) indicating that inhaled medication is generally deposited away from the areas of inflammation. This observation is useful when designing medical treatment of lung diseases. Furthermore, particles with diameters from 1 μm to 10 μm are shown to be mainly deposited on the lower airways, whereas particles with diameters of 20 μm and 30 μm are mostly accumulated in the upper airways. As a result, the current analysis indicates increased DF levels in the upper airways when the particle diameter is enlarged. Additionally, when the particles density increases from 1000 Kg/m3 to 2000 Kg/m3, the DF is enhanced on every generation and for all cases investigated herein. The results obtained by our simulations provide an accurate and quantitative estimation of all important parameters involved in lung modeling. Conclusions: The treatment of respiratory diseases with inhaled medical substances can be advanced by the clinical use of accurate CFD and FPT simulations and specifically by evaluating the deposition of inhaled particles in a regional oriented perspective in regards to different particle sizes and particle densities. Since a drug with specific characteristics (i.e. particle size and density) exhibits maximum deposition on particular lung areas, the current study provides initial indications to a qualified physician for proper selection of medication.
Lalas, S. Nousias, D. Kikidis, A. S. Lalos, G. Arvanitis, C. Sougles, K. Moustakas, K. Votis, S. Verbanck, O. Usmani, and D. Tzovaras, “Substance deposition assessment in obstructed pulmonary system through numerical characterization of airflow and inhaled particles attributes,” To appear BMC Med. Informatics Decis. Mak , 2017.